“High Demand for Breast Implants, Yet Complications Remain a Concern”
Many women worldwide undergo breast augmentation each year, with the majority being satisfied with the outcomes. However, some women may find themselves displeased with the results of their initial procedure or notice changes in their breast shape over time due to unforeseen complications.
Commonly seen deformities can be categorized in two groups:
- Implanted Breast Shape Deformities
- Late Breast Implant Complications.
Implanted Breast Shape Deformities
Displacement or improper implant position that can happen in early or late period after breast implantation for different reasons which can affect the appearance of the breasts, causing them to look asymmetrical or unnatural and without or with limited symptoms they complain of. It is vital to address these concerns, as they can greatly affect a patient’s self-esteem and overall satisfaction with their breast augmentation. However, from a medical perspective, these issues can be treated conservatively at least for a while if the patients are not concerned about them. These include:
- Implant displacement & Malposition
-
- Double bubble breast implant deformity.
- Bottoming Out of Breast Implant
- too high (overriding of breast implant)
- too far to either side of the breast (lateral displacement ) or
- too close (Symmastia)
- Flipping of breast implant
- Rippling Or Wrinkling of Breast Implant
- Implant Deflation, Leakage or Rupture
- Water-fall Breast Implant Deformity
- Breast Animation Deformity
- Galactorrhoea
Breast Implant Related Complicaitons
- Breast implant capsular contracture
- Late breast implant seroma
- Breast Implant-associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
- Breast Implant Illness (BII)
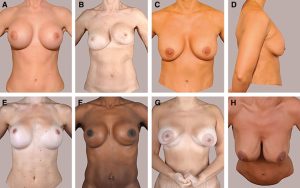
Complications of breast implant documented during physical examination: A, late onset seroma, right breast; B, capsular contracture, Baker grade IV, left breast; C, bilateral waterfall deformity; D, bilateral waterfall deformity; E, bilateral bottoming out; F, left sided double bubble deformity; G, bilateral animation deformity; H, bilateral rippling.
Double-Bubble Breast Implant Deformity
The term “double-bubble” refers to a specific shape that occurs when the breast implant settles below the old inframammary fold (the crease where the breast meets the chest wall). This creates the appearance of a double contour, with the implant positioned lower than the natural breast tissue. This complication can be caused by various factors, including inadequate pocket dissection or improper releasing a constricting band that the patient has it preoperatively as in tuberous breast causing double bubble deformity that appear in early after surgery.
The patient notice the double bubble effect like having two breast mounds because the breast implants don’t settle properly
Surgical correction, which may include revising the inframammary fold, adjusting the implant pocket, or exchanging the implant for a better fit. Mild cases can be corrected successfully with fat grafting with shorter recovery time.
This complication requires a breast revision by an experienced cosmetic surgeon
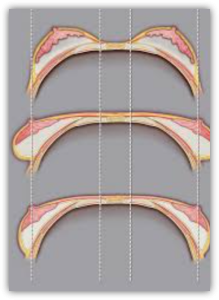
Bottoming Out Breast Implant Deformity
Breast implant bottoming out is a potential complication that can arise after undergoing breast augmentation using breast implant. It refers to a situation where the breast implant descends further on the chest wall than intended, resulting in an abnormally low placement and stretching of the skin from the nipple to the fold, although the breast crease is in perfect position. This downward displacement causing them to protrude excessively from the lower breast area causing unbalanced or disproportionate appearance of the breast, compared to the expected teardrop or round shape of a breast implant.
Moreover, the nipple’s position may change as the implant descends lower on the breast mound, resulting in an upward-pointing rather than facing forward or central.
This complication occurs when the natural breast tissue fails to provide adequate support for the implant, or the implant is too big for the breast. Over time, gravity, along with factors such as the size and weight of the implant, weakens the breast tissue, stretching the skin and underlying tissue causing the implant to shift downwards below its natural original position causing breast asymmetry if it happen on one side and an unnatural appearance.

Bottoming out ruins patients’ expectations. Signs and symptoms that implants have bottomed out include:
- Nipples are pointing upward, and sit higher in the breast
- A visible inframammary scar. After a successful breast augmentation, the inframammary scar isn’t obvious, as it’s hidden in the fold of your breast. If the scar has risen on the chest, it’s a sign of the bottoming out effect.
- Excessive visibility or palpability of the implant
- Patient feels discomfort or pain in her lower breast. When the implant slips down to the lower breast, the patient may experience pain and pressure in the area.
- Patients see a loss of upper breast volume. With the implants drooping to the lower part of the breast, the upper part suffers a loss of volume.
Surgical Correction: Reinforce the lower pole of the breast and reset the lower pole skin to shorten the distance between the nipple and the fold, Sometime my need to use a synthetic mesh internally to support the implant because the breast tissue too week to support the implant or switching to a smaller implant size.
The Differences Between Double Bubble and Bottoming Out:
I’m bottoming out are both complications of a breast augmentation, but they are not the same thing the key differences that distinguish each include:
- Bubble refer to a situation where the breast tissue falls below the breast implant or your tissues push them up higher than they should be
- bottoming out involved the implants sagging far below the natural in from America Greece
- double bubble mostly occurs with large implants
- double bubble can occur even if the breast enhancement didn’t include a breast lift
- bottoming out mostly occur because of poor citra cultural support for the implant
Important to Know
It is important to note that both complications bottoming out & double-bubble breast implant complications can occur separately or in combination, depending on individual factors and surgical techniques used.
Over-riding of breast implant (high breast implant malposition)
It is one of the potential complications that can arise shortly after a breast implant procedure or later. It may result in asymmetry if it affect one side only as the affected breast may appear higher, with the implant positioned closer to the collarbone than the other breast. This deformity can distort the appearance of the breasts and significant emotional distress and self-consciousness for the individual who has undergone the procedure.
In early period after the surgery, it can happen due to swelling or implant displacement (hematoma or seroma should be excluded). Proper management and follow-up will be needed. If it sustained, It can be due to improper pocket dissection to let the implant settle in right place comfortably.
Rrevision surgery will be needed if the issue not solve by conservative management as using bra binder. If this deformity appear as a late complication after months or years, it occur due to capsular contracture, a condition where the scar tissue around the implant tightens and hardens, causing varying degrees of distortion and discomfort. Capsular contracture can occur in one or both breasts and can range from mild to severe (READ CAPSULAR CONTRACTURE)
Lateral Displacement of Breast Implant (Malposition of the Implant to the Sides )
Lateral fullness of the breasts (the edge of the breast that sits closest to the arm) is not always a bad thing. Some degree of fulness here contributes to a curvier and perhaps a more voluptuous breast contour. Unfortunately, this lateral displacement could become a big issue if the implants displaced far out of the side, leaving little to no implant on the anterior projection. This also creates an abnormal gap between the breasts.
This displacement is particularly noticeable when one is lying on their back. Though this same appearance may be seen with non-augmented droopy breasts, it is not a very desirable look for those who have had a breast augmentation.
Malposition of the implant to the side occurs when the implant shifts laterally. These complications can lead to breast asymmetry and an unnatural appearance. It happen either
- Big pocket dissection
- Selected implant that are too large and/or too wide for one’s anatomy
- Decreased breast skin elasticity often associated with disproportionately large implants
- Lack of appropriate breast support with a bra
- sleeping on one side in early stage of the recovery without any support. Revision surgery is often necessary to reposition the implants and construct the pocket
- Suboptimal surgical technique
- Trauma
Revision surgery is often necessary to be done by highly expert cosmetic breast surgeon to reposition the implants and construct the pocket
Symmastia

Symmastia occurs when the implants have been placed too close to each other and the tissue that separates them is stretched or merged. The skin lifts off the underlying sternum (breastbone). This causes a patient’s breast to connect in the midline, giving them of one breast (uniboob).
If Symmastia occurs shortly after a breast augmentation procedure, it can sometimes be successfully treated with postoperative intermammary compression by using a special bra that pushes the cleavage skin against the breastbone held in place like this, the skin will sometimes adhere to the bone producing a permanent correction.
Most instances of symmastia require surgical correction. Various options are available for breast reconstruction in such cases, including shifting the implant to a submuscular pocket or opting for a smaller implant size if the current one is too large for the pocket. All of these options aim to close off the excessive inner edge of the pocket, although the specific method of closure may differ among them.
Rotation of the breast implant (Flipped Implant)
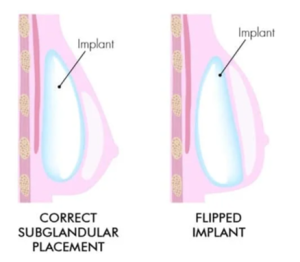
Rotation of the breast implant (Flipped Implant) : It is the situation where an implant rotates front to back ( or anterior to posterior) 180 degree within the breast pocket. This can occur due to factors such as implant size, placement, or movement of surrounding tissue.
This movement can cause asymmetry, discomfort , and affect the over all appearance of the breasts.
While it is a relatively uncommon occurrence, rotation can result in asymmetry or alter the desired breast shape. Surgeons often address this issue through follow-up visits to reposition or stabilize the implant, ensuring optimal aesthetic outcomes and patient satisfaction.
Rippling or wrinkling of the breast implant

Rippling or Wrinkling: Patients often feeling their implants, but the feeling is different with visible rippling as in some cases, patients may notice visible rippling or wrinkling of the breast implants. The most common cause of rippling, however, is the fact that patients do not have adequate coverage over their breast implants, and this is most common in thin patients with low percentage body fat. This can affect the aesthetic appearance of the breasts.
Options for addressing rippling may include fat grafting which represent the most successful option, or implant size adjustment, or using a different implant type.
Implant deflation, leakage or rupture
 An implant rupture refers the tearing or leakage of the implant shell. This can occur due to trauma, implant age-related wear and tear, or manufacturing defects. which can either take place silently (without symptoms) or present with breast pain, changes in breast shape, or asymmetry.
An implant rupture refers the tearing or leakage of the implant shell. This can occur due to trauma, implant age-related wear and tear, or manufacturing defects. which can either take place silently (without symptoms) or present with breast pain, changes in breast shape, or asymmetry.
Saline implant deflate rapidly when it ruptured, while silicone gel implants display subtle changes in shape or hardness.
Surgical removal of the implant with capsulectomy is highly recommended with replacement of the breast implant or replace the implant with fat transfer or breast tissue adjustment with mastopexy with or without lipotransfer.
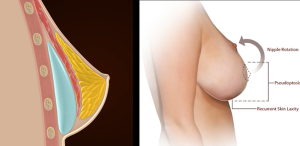
Waterfall Breast Deformity or Snoopy Dog Breast Deformity
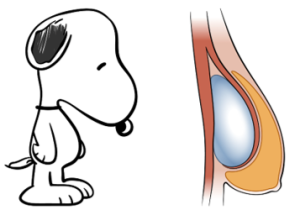
Waterfall breast deformity, is a condition that affect the implanted breast causing an unnatural breast looking due to downward displacement of breast tissue below the position of the implant, as in this deformity the breast implant is in proper position, but the breast mound slides below result in less-than-ideal aesthetic outcome & unsatisfied patients. This gives the appearance of a dad looking snoopy dog with the nose pointed towards the ground. It also called water fall deformity, due to the appearance of breast tissue spilling over the breast implant like a waterfall.
Signs and Symptoms: It is identifiable through specific visual and physical indicators. associated with this condition include:
- gap between the implant that located at the upper pole and the ptotic breast tissue.
- low nipple-areolar complex causing an unnatural appearance.
- lower portion of the breast may sag or hang causing the “waterfall” shape.
Surgical correction :may indicate implant exchange plus mastopexy (breast lift) to adjust the breast tissue and nipple-areola complex in more proper and aesthetically pleasing position.
In some cases, the internal bra technique can provide additional support to the implants and breast tissue. This can involve using sutures or surgical mesh to secure the implant in a desired position, preventing the recurrence of the gap between the implant and breast tissue.
Breast Animation Deformity BAD
Breast animation deformity (BAD), It has been reported to occur after submuscular implant placement following breast augmentation. It is a condition in which the shape of the augmented breast changes or is distorted during contraction of the major pectoralis muscle.
The distortion may lead to varying degrees of widened cleavage, and upward or superolateral implant malposition and asymmetry.
Despite its apparent impact on patients’ quality of life, BAD has only recently become a topic of general concern.
Various methods of treating BAD have been investigated, including neuromodulating injections into the pectoralis major muscle, selective nerve transection, reoperation with a muscle-splitting technique, and repositioning of the implant to a prepectoral position with or without fat grafting.
Galactorrhea
Galactorrhoea, the uncommon complication after breast enlargement using breast implant, which is the spontaneous flow of milk from the breast unrelated to pregnancy or breastfeeding. It can also represent as Galactocele, which consists of milk accumulation inside the implant pocket mostly without nipple discharge.
First two galactorrhoea cases after using breast implant for augmentation, was reported 1971 while, first galactocele case reported 1979.
Risk factors have been well reported in the literatures however, the exact cause remains unclear & not well understood but mostly, correlated with increase the prolactin hormone. It is usually caused by hormonal imbalances, medications, thyroid disorders, pituitary tumors, or other medical conditions affecting the endocrine system.
Treatment: treatment algorithm is conservative.
Important to Note
Patients contemplating breast implant surgery should ensure to inform their surgeon if they experience nipple discharge, even if they have no recent history of pregnancy or abortion, or if they have a history of secondary infertility, as these factors may be linked to elevated levels of the hormone prolactin.
Important to Remember
It is important for patients considering breast implant surgery to be aware of the importance to inform your surgeon if you have any discharge from nipple or if you have a concern about it as it better to do thorough investigation about it before plan for breast implant surgery.
Late Breast Implant Complications

Complications related to the Breast Implant
The second group of complications is collectively known as “late breast implant-related complications”, these complications are of utmost importance as they can have long-term effects on the patient’s well-being. It is crucial to consider these complications seriously to ensure the patient’s ongoing health and happiness with their breast implants. The risk of experience these complications is low. As the lifespan of the breast implants increases, so does the risk of it. It includes:
- Breast implant capsular contracture
- Late breast implant seroma
- BIA-ALCL
The risk of experience these complications is not common but as the lifespan of the breast implants increases, so does the risk of complications.
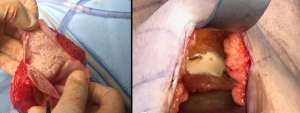
Capsular Contracture
Breast implant capsular contracture is a potential complication that can occur after breast augmentation surgery. It is characterized by the formation of a hardened scar tissue capsule around the breast implant, leading to varying degrees of breast firmness, pain, and distortion in shape.
Some people tend to develop thick scar tissue after any kind of penetrating skin injury, while others can sustain deep cut and develop only subtle scarring that fades over time. Another good example of this difference is the way some women will develop severe stretch marks during pregnancy no matter what they do to prevent them, whereas other women emerge from pregnancy nearly stretch mark-free. Additionally, everyone’s immune system respond differently to stimuli, and some patients’ immune systems react poorly to medical implants.
Causes:
The exact cause of capsular contracture is not fully understood, but several factors have been suggested to contribute to its development. These factors may include:
- Implant Type: Older generation silicone implants have been associated with a higher risk of capsular contracture compared to modern silicone gel-filled implants.
- Bacterial contamination: In some cases, bacterial contamination during surgery or in the surrounding breast tissue may trigger an immune response, leading to excessive scar tissue formation.
- Bleeding or hematoma: Hematomas, which are blood collections around the implant, can increase the risk of capsular contracture.
- Implant rupture or leakage: Silicone gel or saline leakage from a damaged implant may contribute to inflammation and the development of capsular contracture.
- Implant surface texture: Textured implants were initially introduced to reduce the risk of capsular contracture, but recent studies have shown a potential association between textured implants and a higher risk of developing severe capsular contracture.
Grades: Capsular contracture is typically categorized into four grades based on the Baker classification system:
- Baker I: The breast is soft; implant is not palpable
- Baker II: The breast is solid; implant is palpable but not visible
- Baker III: The breast hardened; implant is palpable and visible
- Baker IV: The breast is hard, disformed, and painful; implant is palpable and clearly visible
Severe capsular contracture may require surgical intervention and implant removal.
Treatment options: for capsular contracture depend on the severity of the condition. They may include:
- Non-surgical interventions:
- Massage Techniques: Regular and appropriate breast implant massage can help prevent or alleviate early signs of capsular contracture.
- Medications: Prescription medications like Singulair (Montelukast Sodium) have shown promising results in reducing the incidence and severity of capsular contracture.
- Surgical interventions:
- Capsulotomy: This procedure involves making incisions in the scar tissue to release the tightening and allow for better implant movement. (Recently, this option has become less preferable due to the update regarding BIA-ALCL, and there have been many opinions against it).
- Capsulectomy: The removal of the entire capsule is considered in severe cases of capsular contracture, coupled with implant replacement. Due to correlation of breast implant capsular contracture with the incidence of BIA-ALCL, researcher highly recommend full capsulectomy as possible to avoid the disease that could happen even after implant explantation if the capsule left behind.
- Changing Implant Size or Type: In some cases, replacing the implant with a different size or type may be recommended to minimize the risk of recurrence.
- Implant Pocket Change: Switching the implant pocket placement (e.g., from subglandular to submuscular) can help reduce the risk of future capsular contracture.
Important to Remember:
While capsular contracture remains a potential complication of breast augmentation surgery, understanding its causes and available treatment options empowers individuals to make informed decisions about their health. If you experience any symptoms of capsular contracture, it is important to consult with your plastic surgeon, who can provide a thorough evaluation and guide you towards the most effective treatment option.
Late Idiopathic Breast Implant Seroma
an uncommon complication that can occur after breast implant surgery, where the fluid accumulate around the implant. It may cause swelling, pain, and a change in the shape of the breast when the case is severe type which can be a distressing issue for many women. While seromas typically occur shortly after implantation, there are cases where it develops years later, giving rise to late idiopathic breast implant seroma with risk of developing is rang between 0.05%- to 0.1% for women with textured surface breast implants. It is a unique challenge for both patients and healthcare providers. Unlike seromas that occur shortly after surgery, the exact cause of late seromas is often unclear, hence the designation “idiopathic” This feature can make diagnosis and treatment more complex since there might not be a clear triggering event or underlying issue to address.
Causes: While the specific causes of late idiopathic breast implant seroma are still not fully understood, there are several theories that researchers and medical professionals consider. Some of these potential causes include:
1.Chronic inflammation: Long-term low-grade inflammation around the breast implants might contribute to the formation of seromas. Inflammation can be triggered by various factors, including the body’s immune response to the implant.
- Capsular contracture: Capsular contracture occurs when the scar tissue (capsule) forming around the breast implants tightens and constricts. It is thought that the tightening of the capsule can potentially lead to fluid accumulation.
- Trauma or injury: Physical trauma or injury to the breast area, even several years after implantation, might cause fluid buildup due to the disruption of tissues.
Treatment Options: The management of late idiopathic breast implant seroma involves a multidisciplinary approach, including consultation with plastic surgeons, radiologists, and medical oncologists. Here are some potential treatment options that may be considered:
- Aspiration: In mild cases where the accumulated fluid isn’t causing significant discomfort or complications, the fluid can be drained through an ultrasonography-guided needle aspiration procedure. This may provide temporary relief and the important is to send the fluid for enzyme-linked-immunosorbent serologic assay for CD30 test to exclude BIA-ALCL.
- Anti-inflammatory medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to help reduce inflammation around the implants and potentially reduce the recurrence of seromas.
- Surgery: In more severe or recurring cases, surgical intervention may be necessary. The options might include removing the affected implant, replacing it with a new one, or removing both implants if deemed necessary.
- Observation: In some instances, a “watch and wait” approach might be adopted, particularly if the seroma is small in amount, asymptomatic, and not causing any significant aesthetic or functional impairment.
Important to Remember
Late idiopathic breast implant seroma is a complex condition that requires a thoughtful approach to diagnosis and treatment as the risk of its correlation with BIA-ALCL has been mentioned in many studies. So, if you suspect that you have a late seroma, it is crucial to consult with your plastic surgeon for a thorough evaluation. Together, you can explore the available treatment options and determine the best course of action to address your specific situation.
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)
is a rare form of non-Hodgkin lymphoma, primarily associated with textured breast implants.
Causes and Risk Factors:
BIA-ALCL is believed to result from a complex interaction between genetic predisposition, chronic inflammation, and the presence of textured breast implants. Textured implants are thought to trigger a chronic immune response, leading to the development of BIA-ALCL in susceptible individuals. The risk of BIA-ALCL appears to be higher with textured implants compared to smooth implants.
Understanding the Frequency and Occurrence:
BIA-ALCL is an extremely rare condition. Current estimates suggest an incidence ranging from 1 in 3,817 to 1 in 30,000 patients with textured implants, highlighting its overall low prevalence. Thus, the risk of developing BIA-ALCL post-breast implant placement is considered to be very low.
Presentation and Diagnosis: Patients with BIA-ALCL typically present with late-onset fluid collection (seroma) around the implant, usually between two to twenty-eight years after implant placement. Symptoms may include breast swelling, pain, or capsular contracture. A thorough diagnostic evaluation, involving imaging techniques, fluid analysis, and histopathological examination of tissue samples, is necessary to confirm BIA-ALCL.
Treatment: The primary treatment for BIA-ALCL is the removal of both the implant and the surrounding capsule (total capsulectomy). In most cases, this is sufficient to achieve complete remission. If the disease has advanced, additional treatments such as chemotherapy or radiation therapy may be recommended. Prognosis for BIA-ALCL is generally favorable, with a high overall survival rate.
Ongoing Research Efforts: Given its rarity, ongoing research aims to further understand the pathogenesis, risk factors, and optimal treatment strategies for BIA-ALCL. Scientific and regulatory bodies are actively monitoring the safety and efficacy of breast implants, including the association with BIA-ALCL. Research efforts are focused on improving diagnostic techniques and exploring the role of genetic factors in predisposing individuals to BIA-ALCL.
Breast Implant Illness (BII)
Breast augmentation with implants is one of the most commonly performed cosmetic procedures worldwide, with millions of individuals choosing to undergo this surgery each year. While breast implants are generally considered safe and effective, a subset of individuals develop a range of nonspecific symptoms following implantation, collectively known as Breast Implant Illness (BII).
Breast Implant Illness (BII) is a complex phenomenon characterized by a constellation of symptoms that affect individuals with both silicone and saline breast implants. Despite the ongoing controversy and limited scientific consensus surrounding BII, recent studies have shed light on the potential mechanisms underlying this condition and its clinical manifestations.
The symptoms associated with BII may include fatigue, joint pain, cognitive difficulties, and autoimmune-like symptoms, among others. The exact prevalence of BII remains uncertain, partly due to the lack of standardized diagnostic criteria and the variability of symptoms reported by affected individuals.
The pathophysiology of BII is not yet fully understood, although several potential mechanisms have been proposed. One prevailing theory suggests that the immune system may play a central role in the development of BII. It is hypothesized that chronic inflammation triggered by the presence of breast implants could lead to dysregulation of the immune response, resulting in the systemic symptoms observed in affected individuals. Additionally, the release of silicone or other implant-related compounds into the surrounding tissues may elicit an inflammatory response and disrupt normal physiological processes, further contributing to the development of BII
Diagnosing BII remains a challenge due to the lack of specific biomarkers or definitive tests for the condition. Clinicians often rely on a thorough clinical history, physical examination, and exclusion of other potential causes of symptoms to make a diagnosis of BII. Furthermore, the nonspecific nature of BII symptoms can overlap with other common conditions, making it difficult to differentiate BII from other health issues. Despite these diagnostic challenges, increasing awareness of BII among healthcare providers and the general public is essential to ensure timely recognition and appropriate management of affected individuals.
In conclusion, Breast Implant Illness is a multifaceted condition that continues to pose diagnostic and therapeutic challenges for healthcare providers. While the pathophysiology of BII remains unclear, ongoing research efforts are crucial to elucidate the underlying mechanisms and improve diagnostic strategies for this condition.
Enhancing the knowledge and awareness of BII among clinicians and patients is essential for facilitating early detection and management of affected individuals. Further studies investigating the relationship between breast implants and systemic symptoms are warranted to advance our understanding of BII and improve patient outcomes.
Important to Remember
- It is important for patients considering breast implant surgery to be aware of the potential risks associated with breast implants and to engage in informed discussions with plastic surgeon. Routine follow-up examinations and immediate reporting of any concerning symptoms are crucial. Regulatory agencies and professional societies continue to update guidelines and recommendations based on emerging evidence to ensure patient safety.
- Monitoring Implant ConditionIt’s essential to maintain regular check-ups with your plastic surgeon to monitor the condition of your implants. Dr. Kazzaz offering her patients complimentary annual clinical check up for the implant and the capsule situation. In case of any clinical suspicions, an imaging techniques, such as breast ultrasound may be needed to rule out any suspension. An advanced radiology imaging as MRI scans, are recommended globally by some health authorities to check for silent ruptures in silicone implants, typically starting around the fifth-year post-surgery and every two years thereafter.